Binocular Vision Q&A: Case 1
Questions:
- Why is the VA so reduced with such a small Rx? Is this due to the BV problem? Should the patient be referred due to the VA? Should we do additional tests to rule out other causes, such as visual fields? Would you expect the VA to improve following the exercises?
- What would be the expected normal positive fusional reserves?
- What target would you use for near cover test following cycloplegic? Or do you need to wait until the cycloplegic effects worn off?
- As we have a high rate of non-compliance with exercises, what would you do if the patient returns and hadn’t been doing them much? Or if it appears they are unlikely to do them?
- If the accommodation was reduced would a reading add help? Would you prescribe base-in prism for near tasks in this case? Would your management differ for an adult compared to a child?
- Should the patient be referred for the non-BV reasons (the coloured flashing lights?) and suspect migraine?
Answers:
1. Why is the VA so reduced with such a small Rx? Is this due to the BV problem? Should the patient be referred due to the VA? Should we do additional tests to rule out other causes, such as visual fields? Would you expect the VA to improve following the exercises?
- First of all a quick reminder – this appointment was focussed on the binocular vision issues. The patient had recently undergone a full eye examination and ocular health check, therefore any obvious causes will have been picked up, any further investigations carried out and the patient referred if required.
- In cases of decreased convergence and decompensating exophorias, we would expect reduced near visual acuities.
- The cycloplegic refraction was done to check for any uncorrected refractive error. There could be uncorrected hyperopia. The patient would have used their accommodation to compensate for this, but had reached a point when they were no longer able to do so, leading to decompensating exophoria. This is possible with even small amounts of hyperopia. It is difficult to say whether this is true in this patient – we would expect an even smaller amplitude of accommodation.
- Other factors to consider include: time of day of appointment and the patient’s fatigue level; difficulty in reading letters on the VA chart (consider trying another chart – if possible); patient motivation to engage with test.
- At the end of the first appointment there were still unanswered questions about the patient’s VA, but there was nothing to suggest that a referral was required at this stage.
- The first course of action is to manage the symptoms and improve control of the phoria. A careful check of VA at the follow-up appointment is required. Follow-up investigations with visual fields for example could be considered.
2. What would be the expected normal positive fusional reserves?
The values for normal limits of fusional reserves will vary depending on the source of information. Here are a few examples:
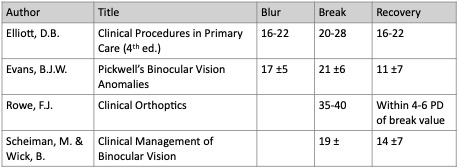
There is limited research in this area and many practitioners are guided by their own clinical experience. In our clinic, we use a break value of 35-40∆ as the norm, but it is probably more important to judge whether the patient’s fusional reserve is acceptable or not, based on their individual clinical data and in particular if they are experiencing symptoms or not.
3. What target would you use for near cover test following cycloplegic? Or do you need to wait until the cycloplegic effects worn off?
You could use an aspect of one of the pictures on the fixation stick or a larger letter. We do not require an accommodative target at this stage.
4. As we have a high rate of non-compliance with exercises, what would you do if the patient returns and hadn’t been doing them much? Or if it appears they are unlikely to do them?
There is no easy answer to non-compliance! We tend to give our patients a couple of chances, but adopt a more direct style of communication! Some patients do not remember all the instructions from the first visit, so a close follow-up allows us to correct any misinterpretations. In some cases it is useful to put the consequences into the context of the patient’s daily routine to help them understand that they may not be able to do a certain hobby or read or similar, because their symptoms will cause them discomfort.
To try and avoid these problems arising, it may be useful to give the patient a written instruction or suggest that they have a background distraction, such as a 2 to 3-minute piece of music that they listen to whilst doing the exercises, or perhaps other ways in which the exercise can be fitted into their daily routine. Give the patient a series of interesting fixation targets – not just a pen, so that they have some variety. It may also be useful if a patient has to start off with a larger target but is able to use a smaller target as their binocular control improves.
5. If the accommodation was reduced would a reading add help? Would you prescribe base-in prism for near tasks in this case? Would your management differ for an adult compared to a child?
Spherical or prismatic management could be considered. In this case it would be a second line of management – if the exercises had not been successful or if the patient was struggling to do them. In cases where the patient has a more remote point of convergence, for example 50cm, then some base-in prism may help them initially, but in most cases, this would not be a permanent part of their prescription.
In this case, the accommodation should improve once control of the phoria improved. In cases where the amplitude of accommodation was poor and the dynamic retinoscopy result indicated a noticeable lag, then an add could be considered.
In this case, the management would be the same regardless of the patient’s age.
6. Should the patient be referred for the non-BV reasons (the coloured flashing lights?) and suspect migraine?
The patient should be referred for any non-BV reasons, if it is justified. If the patient reported that they could not manage the migraines, then it would be sensible that they speak to their GP in the first instance.